Note: for those of you who are new to the "insulin pump game" and are not sure what some of the terms are that I am using, please see a
previous post of mine.
For those of you who have lived with your insulin pump for quite a time you know this procedure all too well. For those of you looking at getting an insulin pump what follows is a description as to what you will be doing every third day (at the most). This is an extremely long post, however it will take longer to read it than it actually takes you to change your infusion set...just being thorough! (Once again, remember I am NOT giving this as professional advice, but just my personal experience. Nothing I say should circumvent what your diabetes educator will tell you....I am just giving you an idea of what it is like.)
What you need:
- insulin pump
- insulin (a rapid acting one)
- reservoir
- tubing (unless you have a tubeless pump)
- infusion set
- alcohol swab
- Polysporin (or some other antibiotic cream) - optional
- band-aid - optional
- cannula inserter - optional
I use a Medtronic MiniMed pump with a Silhouette infusion set. Therefore my post will have details about this, but all insulin pumps will have similar steps.
The recommendation is that you change your infusion set every third day, and if you are lucky, that will coincide nicely with the amount of insulin your reservoir can hold, so you are changing everything at the same time. One needle every third day is a heck of a lot nicer than up to 12 or more injections over three days on a traditional syringe treatment.
1. The first thing I have to do is take off the the infusion set that is on/in me. In the picture you will see that I can unhook the tubing from the infusion set.
At this point I now have to take the infusion set out of my stomach (my preferred location). While the set is attached to me with an adhesive, it fortunately does not leave a sticky residue. When I peel the infusion set off, it pulls the plastic cannula out as well. Extremely rarely will there be any blood. (Of course the first time I tried it with my nurse educator, I bled for a few minutes! Talk about a bad start!) To reduce scarring, I use a dab of Polysporin before covering it with a band-aid. The cannula goes in the garbage.
2. I then have to remove my reservoir from my insulin pump, which is done with a simple twist and another twist to get the tubing off of the reservoir. At this point I also have to "rewind" my pump, so the plunger that pushes the insulin out of the reservoir rewinds back into the pump (this is done with a couple quick button presses on my pump).
3. I am now ready to start from scratch and get the new supplies ready to go. I start by getting my reservoir full of insulin. In the picture below you will see the reservoir as it comes out of the box. It has top, middle, and bottom sections. The top (blue) attaches to your vial of insulin. The bottom is how you pull back the rubber section inside the reservoir that holds the insulin. The middle section is the reservoir itself, which goes into your insulin pump when it is filled with insulin.
You should pull back and forth (while twisting) on the bottom part so that the lubricant on the rubber inside the reservoir can loosen up. Apparently it helps so that there is less pressure on your insulin pump to do the work, which could burn the motor over the course of a few years.
4. Before attaching the blue part to the insulin vial I like to pull back air into the reservoir to push into the insulin vial (much like with traditional syringes, to maintain air pressure inside the vial). While the blue part is a "venting cap", I find it much easier to push air into the vial myself. You then simply pull back slowly on the bottom of the reservoir to pull back insulin into the reservoir, ensuring to keep it vertical, so all bubbles go to the top. You then may have to go back and forth a few times (possibly tap on the reservoir a little) to get all the bubbles out.
5. When the reservoir is full of insulin (no air), you can turn the vial right-side-up, and twist the reservoir off of the blue part (venting cap). The bottom part of the reservoir also twists off of the reservoir itself.
6. At this point you can attach the tubing to the reservoir (where the venting cap was) with another simply twist. You can also insert the reservoir into the insulin pump and twist it into a locked position.
7. Now you need to get your cannula inside you. There are a number of infusion sites to choose from. You can do it pretty much anywhere you used to inject insulin with a syringe, including your upper arms, thighs, upper buttocks, or your abdomen (my favorite). If you choose to always put the cannula into the same area (i.e. only the abdomen) ensure you rotate around the area so that you do not get a build up of scar tissue, which will adversely affect your insulin absorption.
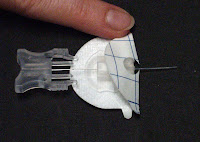
8. Once you have chosen your site, clean the area with your alcohol swab. Let it dry for a few seconds. You can then load your cannula inserter, if you wish to use it. As I noted in a previous post, I tried it a few times and do not like it. I find it much easier to insert the cannula manually, although the inserter (which is basically a spring load device that shoots the cannula into you, much like your finger pricking device) can help getting to harder to reach areas. The cannula (which is the flexible teflon tube that sits inside you) is shown on the left. On the right, you will see how I get the cannula out of the box. It has a needle inside the cannula and has the adhesive around it (the plastic you see in this picture is actually a protective tube that you must remove...it is so you don't prick yourself by accident!).


There are generally two backings to remove from the adhesive, one of which you take off before putting the needle into you (see the picture below to see the raised part of the adhesive which is removed first). Despite my preliminary reservations, the needle with the cannula around it, goes into your body just as smoothly as a regular injection (seriously). You can then ensure the exposed adhesive is applied evenly to your skin. At that point you just have to pinch the two sides of the grey plastic part in the picture on the right and pull the needle out. That leaves the cannula safely inside you. You can then pull off the second backing from the adhesive and ensure the full adhesive is nicely attached to your body.
9. You now have to "prime" your tubing (if you have tubing). Again, with a few clicks on your insulin pump, you will fill the tube with insulin, again so there is no air in there. Next, you affix your tubing to your cannula (see the first picture in step 3.
10. Your final step is to prime the cannula, as that is currently full of air. You simply have to hit one more button on my pump and it pumps in a set amount of insulin, enough to simply fill the cannula with insulin (this amount you will find in your cannula instructions.
Really long post, but it is really a quick process!